
Cold sores, also known as fever blisters, are a common viral infection caused by the herpes simplex virus (HSV-1). According to the National Institute for Health and Care Excellence [1], data reveals that the global prevalence of HSV-1 infection at any site of the body in people aged 49 or below is 67%. Learning the stages of an HSV-1 infection and understanding the process of an outbreak, as well as levels of contagion and duration of an episode, can make controlling the cold sore outbreak much more manageable.
What are cold sores?
Cold sores are small, painful blisters that typically appear on or around the lips, although they can also occur on other areas of the face, such as the nostrils or chin. They are painful and highly contagious.
How are cold sore infections developed?
The infection occurs through direct contact with an active cold sore or by sharing items such as lip balm, utensils, or towels with an infected person. Once the HSV-1 virus enters the body, it remains dormant in the nerve cells until triggered by factors like stress, illness, or sun exposure. Whilst there is currently no cure for HSV-1, the condition is highly treatable.
What are the 5 stages of a cold sore?
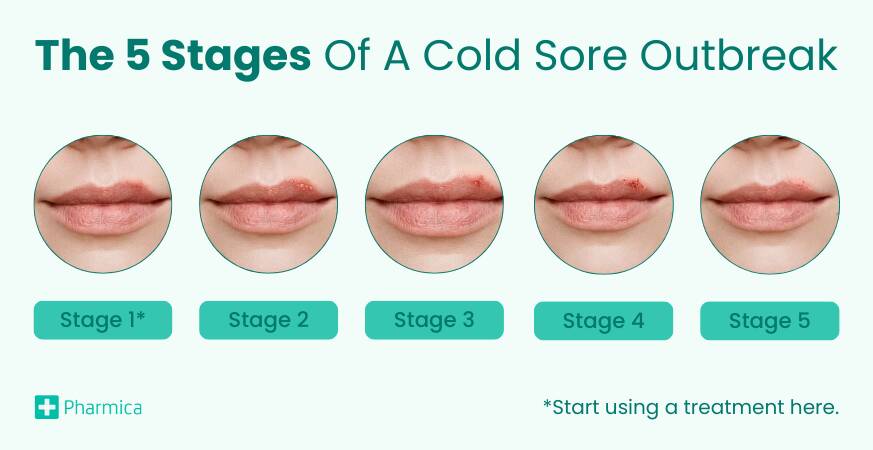
Stage 1
Duration: Day 1-2
Contagiousness: Low
Symptoms: Tingling or itching sensation around the lips or mouth
Experiencing a tingling or itching sensation around the lips or mouth is the first indication that a cold sore outbreak is imminent [2], although there may be no visible signs of a cold sore at this point. It is crucial to use an effective and clinically proven treatment during this stage to minimise the severity and duration of the cold sore.
Stage 2
Duration: Day 2-4
Contagiousness: Moderate
Symptoms: Small, fluid-filled blisters appear, causing pain and discomfort
These blisters are moderately contagious, and caution should be taken to prevent further transmission. The blisters may cause pain, discomfort, and a burning sensation. It is important to avoid touching or picking at the blisters, as this can exacerbate the condition and increase the risk of spreading the virus.
Stage 3
Duration: Day 4-5
Contagiousness: Severe
Symptoms: Blisters burst, releasing a clear fluid and forming painful sores
The fluid inside the blisters is highly contagious, and proper hygiene practices are essential to prevent the spread of the virus. Gently cleanse the affected area with mild soap and water, and avoid sharing personal items such as towels, lip balms, or utensils.
Stage 4
Duration: Day 5-8
Contagiousness: Moderate
Symptoms: Sores dry out and form a crust or scab
The open cold sores start to dry out and form a crust or scab. It is crucial to resist the urge to pick at the scab, as this can lead to scarring and delay the healing process. Keeping the area moisturised with a lip balm or petroleum jelly can prevent cracking and promote faster healing.
Stage 5
Duration: Day 8-10
Contagiousness: Low
Symptoms: Scab falls off, revealing healed skin
The healing process may vary depending on the severity of the outbreak and individual factors. During this stage, the cold sore is less contagious, but it is still important to practise good hygiene and avoid activities that may irritate the healing skin, such as excessive lip movements or exposure to harsh weather conditions.
Treatment for cold sores
By developing an understanding of the five stages of a cold sore outbreak, individuals can effectively manage the condition and minimise the risk of transmission. Prompt intervention during stage one, the appropriate use of treatment options and adherence to preventive measures can help alleviate symptoms, promote faster cold sore healing and reduce the frequency of cold sore outbreaks.
A first-line treatment for HSV-1 are oral antiviral medications, which offer exceptional efficacy and can make cold sores go away sooner in people who are otherwise healthy [3]. Topical creams and patches are also considered to be highly effective at treating cold sores, especially at aiding the healing process of the sores.
The recommended oral antiviral cold sore treatments consist of:
Aciclovir
Aciclovir (also known as Acyclovir) works by preventing the HSV-1 virus from multiplying, which shortens the duration of the outbreak and dampens the severity of accompanying symptoms. This treatment is considered to be the most cost-effective cold sore treatment available.
Valaciclovir
Valaciclovir (also known as Valacyclovir) is a prodrug of Aciclovir, which means it changes into Aciclovir in the body. As a result, it stays in the body for longer and does not need to be taken as often.
Valtrex
Valtrex is the branded version of Valaciclovir which offers equivalent efficacy as they contain the same active ingredient, however, Valtrex is the more expensive of the two.
Cold sore patches and creams:
Zovirax Cream
Zovirax contains the active ingredient Aciclovir. This topical treatment is effective at treating cold sores within 3 days.
Bonjela Cold Sore Cream
Bonjela cold sore cream is a highly recommended alternative which contains the active ingredient UV-Active™. It works to block UV radiation (a known cold sore trigger) thus preventing HSV-1 from multiplying.
Compeed Cold Sore Patch
Compeed cold sore patches provide excellent discretion. They contain hydrocolloid active gel which works to enhance healing and reduce scabbing.
How to prevent a cold sore from spreading
Cold sores are contagious at all stages of an outbreak until it is completely healed. The risk of transmission can be minimised by:
- Not sharing any items which could come into contact with the affected area, for example, lip balms, cutlery or towels.
- Always wash your hands before and after applying topical treatments.
- Not sharing medication with another person.
- Talking to a partner about the condition.
- Avoiding kissing and oral sex.